
Being Prepared for Severe Lows Just in Case
Begin Preparing for the Unexpected
Keeping a fire extinguisher in your kitchen in case of a fire or having an umbrella in your car in case of rain are common ways to plan ahead and protect yourself. So why not also plan ahead for severe low blood sugar? Sometimes, things that are out of your control can lead to a severe low blood sugar event, so begin preparing for the unexpected today.
Consider taking these steps to be ready for a severe low blood sugar event, just in case:
- 1Create an emergency plan
- 2
Carry your medical ID
- 3Keep your glucagon rescue medication with you
- 4Get your caregivers ready to help you in the moments you can’t help yourself
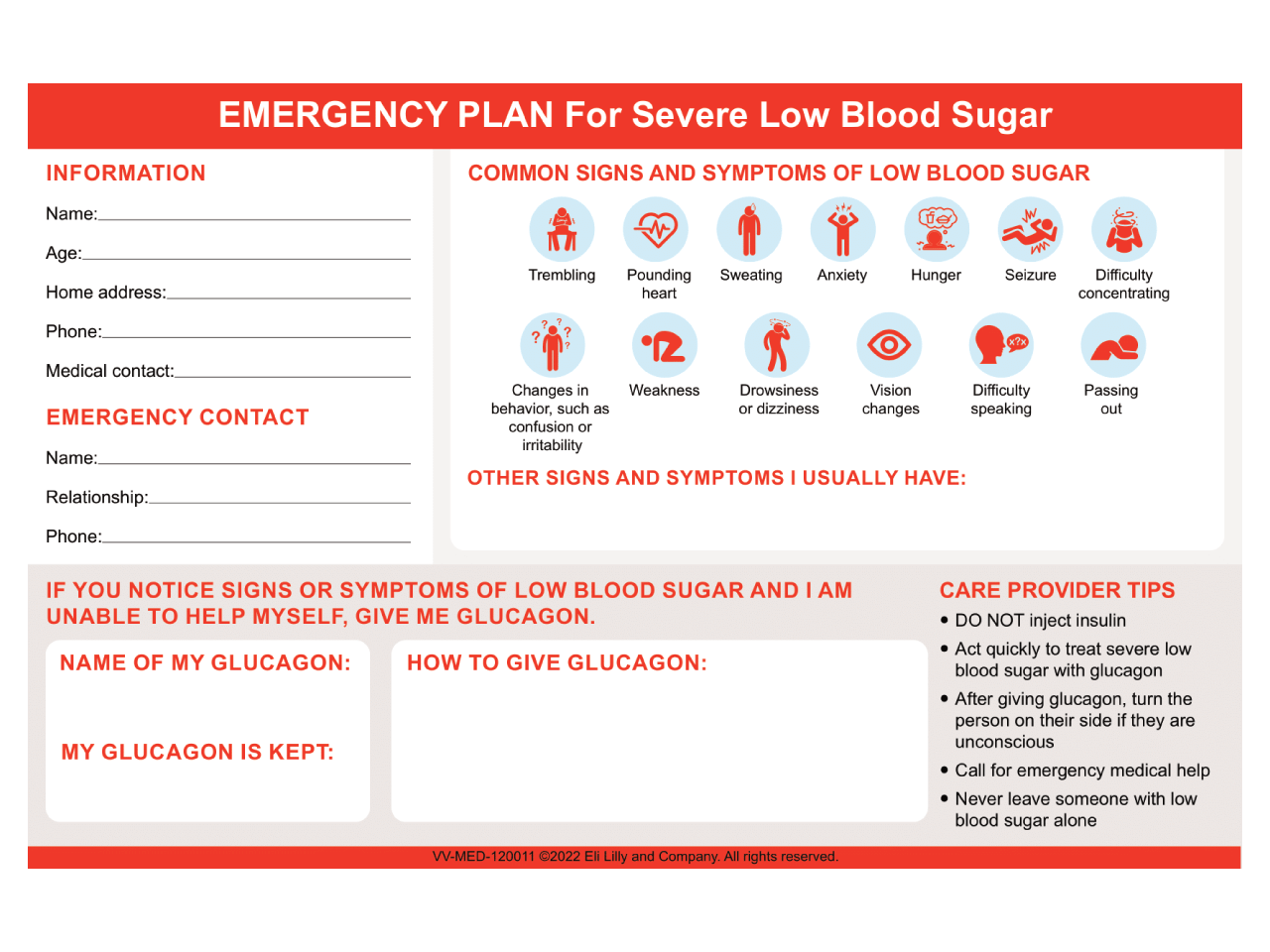
What Is an Emergency Plan?
An emergency plan includes important information that someone else needs to help you during a severe low blood sugar emergency. This includes:
- 1Your name and emergency contact information
- 2YOUR own unique signs and symptoms of non-severe and severe low blood sugar
- 3What to do in a severe low blood sugar emergency, making sure others know where your glucagon medication is and how to use it
What Is a Medical ID?

It’s important for all people living with diabetes to always have a medical ID with them, regardless of the medicines they take. A medical ID provides important information about your health status to those around you. A medical ID is often worn as a bracelet or a necklace, and it includes the following health information:
- The fact that you have diabetes
- Diabetes medicines you take, like insulin
- Any allergies you have
- Your emergency contact information

What Is Glucagon?
Glucagon is a (normal) substance in your body that protects you by telling your liver to release sugar into your bloodstream if the blood sugar becomes too low. People who have diabetes may not have enough glucagon to correct a low blood sugar.
Prescription glucagon can be used when your body does not have enough to bring your blood sugar up to a normal level. There are different types of prescription glucagon, but they all bring your blood sugar levels back up to normal.
When Should Glucagon Be Given?
Glucagon should be given during a severe low blood sugar event, for instance, when you are unable to eat or drink a fast-acting carbohydrate on your own.
Care Provider Tips After Glucagon Is Given
- DO NOT give insulin (it will lower the person’s blood sugar even more)
- DO NOT provide food or fluids (the person may choke)
- Remember to call for emergency services
- Never leave the person with low blood sugar alone
Are You Unsure How to Ask Your Healthcare Provider About Glucagon?
Consider asking some of the following questions:
Things to consider after you have your glucagon medication:
Ask your healthcare provider to teach you and your caregivers how to store and use the glucagon during a severe low blood sugar event.
Keep your glucagon medication with you, as well as fast-acting carbohydrates.
Think about keeping glucagon in the places you stay or visit often. This includes your home and workplace. It could also be a family member's house, school, or your gym
Make sure your caregivers are ready to help you!
Review Your Knowledge
Learn More About Severe Low Blood Sugar
References
- 1Know before the low. Be prepared for low blood sugar. https://www.multivu.com/
players/English/8688551-know-before-thelow/
docs/TipList_1589921095033-1140242936.pdf. Accessed November 21, 2021. - 2American Diabetes Association. Hypoglycemia (low blood sugar). https://www.diabetes.org/
healthy-living/medicationtreatments/
blood-glucose-testing-and-control/
hypoglycemia. Accessed November 1, 2021. - 3Lilly Diabetes Canada. Rescue plan for severe low blood sugar. https://www.whatsyourrescueplan
.ca/pdf/Rescue-Plan-new.pdf. Accessed November 21, 2021. - 4Hormone Health Network. Severe Hypoglycemia. https://www.hormone.org/
diseases-and-conditions/
diabetes/severehypoglycemia. Accessed November 21, 2021. - 5
American Diabetes Association Professional Practice Committee. Diabetes Care. 2022;45(1):S83-S96.
- 6Glucagon for injection [Summary of
Product Characteristics]. Gatwik, West Sussex, United Kingdom: Novo Nordisk.
https://www.medicines.org.uk/
emc/product/1289/smpc#gref. Accessed June 22, 2022. - 7Glucagon nasal powder [Summary of
Product Characteristics]. Fegersheim, France: Lilly France S.A.S.
https://www.ema.europa.eu/en/
documents/product-information/
baqsimi-epar-product-
information_en.pdf. Accessed June 22, 2022. - 8Glucagon injection [Summary of
Product Characteristics]. Marlow, Buckinghamshire, United Kingdom: Tetris Pharma Ltd.
https://www.medicines.org.uk/
emc/product/13093/smpc. Accessed June 22, 2022. - 9Dasiglucagon [Prescribing Information]. Søborg, Denmark: Zealand Pharma A/S.
https://www.accessdata.fda.gov/
drugsatfda_docs/label/2021/
214231s000lbl.pdf. Accessed June 22, 2022.








